Breast milk truly is liquid gold. Your body makes the perfect food for your baby, and pumping lets you give them that milk even when you are not there. Whether you plan to pump occasionally, pump at work after maternity leave, or build a freezer stash, this episode will walk you through how to make pumping easier, more efficient, and less stressful. We’ll cover choosing and using a pump, building and storing your milk supply, navigating pumping at work, and keeping your supply steady.
Listen Now
This episode is made possible with support from our sponsors. I appreciate your support for the brands that help power this podcast.
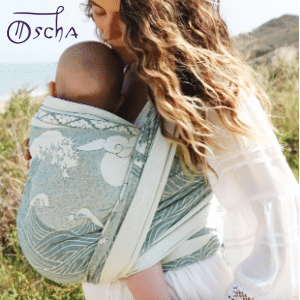
10% off Oscha Slings with the code PREGNANCYPODCAST. From the newborn stage through toddlerhood, Oscha Slings are the most beautiful and comfortable solution for carrying your baby.

The VTech Advanced HQ Max is built for parents who want an easy-to-use, secure monitor without the need for Wi-Fi or apps. With a large 7” screen and crisp, real-time video the Advanced HQ Max is perfect if you want private, no-fuss monitoring with premium features. As the #1 Baby Monitor Brand in North America, VTech is trusted by millions of families. Click here to check out the Advanced HQ Max.

Inito is the first at-home fertility monitor that tracks four key fertility hormones (estrogen, LH, PdG, and FSH) all on a single test strip. Inito is 96% as accurate as a blood test, without the cost, wait time, or hassle of going to a lab. The Inito Starter Pack is available for just $89 with the code PREGNANCYPODCAST.
Become a Pregnancy Podcast Premium member or log in to access all articles and episodes ad-free.
Article and Resources
I support the decisions you make for you and your baby when it comes to feeding. My goal is to provide accurate, evidence-based information and support to help you succeed. You can find all of the breastfeeding resources, episodes, and articles here.
How Long Should Your Baby Get Breastmilk?
The American Academy of Pediatrics’ recommendation is consistent with the World Health Organization and many pediatric associations worldwide. You should exclusively breastfeed your baby for the first six months. At around six months, you should introduce your baby to solid foods while continuing to breastfeed for up to two years and beyond.
Although you introduce solid foods around six months, it takes time for babies to increase consumption of other foods and reduce consumption of breastmilk or formula. For the first year of your baby’s life, they depend on either breastmilk or infant formula as their primary nutrition source.
Understand Why Pumping Matters
If you are breastfeeding without using formula, it can feel like you are constantly tethered to your baby. Pumping gives you the flexibility for your baby to have your milk even when you are not there. This might mean getting out for a few hours to run errands, enjoy time with friends, or return to work. Some parents choose to pump exclusively instead of breastfeeding directly. Pumping can also help you build a freezer stash for future use. In some cases, you can continue feeding your baby breast milk from that supply even after you stop breastfeeding.
Protect Your Milk Supply While Pumping
There is one key principle you need to keep in mind, and that is that milk production works on a demand and supply system. Every time milk is removed, whether by nursing or pumping, your body gets the signal to keep producing at that time. This can be used both to maintain and increase your supply. While it may be appealing to have someone else give your baby a bottle, pumping is most valuable when you genuinely need to be apart from your baby, not to replace a feeding you could do yourself. If your baby gets a bottle at noon, aim to pump around noon to protect your supply. Skipping sessions tells your body that less milk is needed, which will reduce production.
How Much Milk Will Your Baby Need?
When you pump, it is easy to focus on the amount you collect, since you can see it in the bottle. By the end of the first week after birth, most parents produce between 19 and 30 ounces (550 and 875 mL) of milk each day. The average feeding is about 3–5 ounces (90–150 mL), and this amount tends to stay pretty consistent through the first six months. These numbers are specific to breast milk. Because formula is harder to digest and its nutrients are absorbed less efficiently, babies may take larger quantities when fed formula.
Recognize Normal Changes in Pumped Milk
As you start pumping and storing milk, you may notice changes in color, consistency, or smell. Your diet usually causes these variations. They are normal, so there is no need to overanalyze them. You will also notice that breastmilk in a bottle or storage bag will separate into layers as it cools. Breast milk is naturally high in fat, which is ideal for a growing baby, and fattier milk will rise to the top. When warming milk, gently swirl the bottle to mix the layers rather than shaking it. Shaking can break up some of the long-chain fatty acids that are beneficial for your baby.
Choosing and Using Your Pump
Whether you plan to exclusively breastfeed or supplement with formula, it is a good idea to have a breast pump on hand, even if you do not plan to use it daily. Let’s start with your options for pumping milk, how to choose the right pump for your needs, and the basics of getting started.
Choose the Right Pumping Method
There are three main ways to express milk. Hand expression requires no equipment and can be done anywhere. This is a great skill to have for relieving fullness, softening the breast before latching, or collecting small amounts of milk. Manual pumps are simple, portable, and affordable. They work by squeezing a handle to create suction, expressing milk directly into a bottle. These are convenient for occasional pumping but are not a great solution for multiple sessions a day.
Electric pumps are the most efficient. These use a motor to create consistent suction and collect milk into bottles or storage bags. Electric pumps come in two main categories: hospital-grade and home-use. Hospital-grade pumps are the most powerful. They are available in hospitals and due to the cost are usually rented instead of purchased. Home-use electric pumps are designed for long-term personal use and come in a variety of styles, including portable and wearable models. Most of what we will cover here applies to all types of pumps, whether manual, electric, hospital-grade, or hand expression.
Get a Pump Through Your Insurance
In the United States, health insurance plans cover the cost of a breast pump. A fantastic starting place is Aeroflow. This is a company that makes the process of getting a pump through your insurance super easy by working directly with your insurance provider and shipping the pump to you. I have used Aeroflow in the past and highly recommend them. Even if you already have a pump from a previous baby, it is worth getting a new one. Motors can lose power over time, which makes pumping less efficient, and the average pump lifespan is about a year of regular use. If you do not have insurance, talk to your care provider about assistance programs or local nonprofits that provide pumps to parents in need. You can also add a pump to your baby registry, and hopefully, a generous friend or family member will help cover it.
Getting Started with an Electric Pump
Although brands of electric pumps differ in style, they all operate similarly. The flanges are cone-shaped parts that fit over your nipples. They are connected to a motor that creates suction, drawing milk into bottles or bags for storage. Most pumps have tubing connecting the flanges to the motor. You may see some condensation in the tubing, but milk should never enter it. Most pumps plug into a wall outlet, though many also have battery packs or car adapters for flexibility. Wearable pumps operate on batteries and do not require external tubing, the motor is built into the unit that goes in your bra.
Use Pumping Bras or Create Your Own
If you have a wearable pump, you simply slip the units into your bra and pump hands-free. For a traditional pump, a pumping bra allows you to pump both breasts at the same time without holding the flanges in place. This is a big time-saver if you plan to pump regularly. Pumping bras come in many styles, but all have openings that let the flanges fit securely against your breasts with the narrow ends sticking out.
You can also make your own pumping bra. Start with a snug sports bra or spandex bandeau top, put it on, and mark where your nipples are. Remove the bra and cut small holes in those spots, making them just large enough for the narrow ends of the flanges to fit through. You can hem the fabric if you want to prevent fraying, but it is not necessary. This is a temporary item you will only need for a short time, so a DIY version can be a simple and affordable solution.
Setting Up Your Pump
Once you have your pump and accessories it is a good idea to get familiar with your pump before you need it. Read the manual for detailed instructions on operation, cleaning, and care. Before your first use, sterilize all parts that will come into contact with milk, including flanges, bottles, bottle caps, and any connectors. Once you understand how your pump works and the parts are clean, you will be ready whenever you need it.
When to Start Pumping
You might be tempted to practice pumping before your baby arrives. Keep in mind that nipple stimulation triggers the release of oxytocin, which can sometimes start contractions. Some mothers use an electric pump to try to start labor naturally. If you are past your due date and want to try this, it is a good idea to run it by your care provider first.
In the first few days after birth, your body produces small amounts of colostrum. Your mature milk usually comes in on day two, three, or four. Those early days and weeks are a big adjustment as you care for your newborn and navigate breastfeeding. For most mothers, it helps to focus on establishing breastfeeding before adding pumping into their routine. Some situations may call for pumping sooner. You might start earlier if your baby is in the NICU, if you plan to pump exclusively, or if you need to relieve engorgement.
How to Use an Electric Pump
When you first start using your pump, the process can feel a little awkward. It often takes a few sessions to get comfortable and find a routine that works for you. Your surroundings can make a big difference in how productive and comfortable your pumping sessions are. Ideally, you pump in a comfortable, private, and quiet space.
With clean hands, assemble the pump and parts. Position the flanges so your nipples are centered and turn the unit on. Most pumps will mimic a baby’s starting latch with quick, short sucking motions to trigger your milk release (also called letdown). Pumps typically switch to a slower mode after a few minutes or have a button you can press once your milk is flowing to slow the suction. Pumping should not hurt, and you can experiment with adjusting the settings to find a comfortable level. You continue pumping for around 10–15 minutes or until milk flow slows.
Fine-Tuning Your Technique
Once you have the basics down, you can focus on strategies to make pumping faster and more effective. Aim to pump when your breasts feel full, but avoid waiting until you are engorged, which can make milk flow slower, or lead to discomfort and potential issues like plugged ducts.
Many mothers find it helpful to look at a picture or video of their baby to trigger their letdown. Pumping works best when you are relaxed. You can use strategies like deep breathing, listening to music, or looking at photos or videos of your baby. As you pump, experiment with your pump’s speed and suction settings to find what works best for you. Typically, you start with a faster speed to stimulate a letdown, then lower the speed and increase suction for milk expression. Gentle breast massage or compressions during pumping can help stimulate milk flow and increase output. Many mothers find it easiest to focus on compressions on one breast at a time, switching sides periodically.
If you find that your output decreases over time, consider adding sessions. This mimics cluster feeding and can help boost supply. Over time, with patience and practice, you will figure out the techniques and routines that help you pump more comfortably and efficiently.
Cleaning Your Pump Parts
After pumping, you should disconnect the bottles or storage bags and seal them to prevent spills before you do anything else. After removing the flanges from your breasts, leave your pump running for a few minutes to remove any extra condensation from the tubes and pump while you disassemble everything. Any parts that come into contact with milk should be washed. You can handwash everything with a gentle dish soap and warm water, and air-dry it. Having a small dedicated bottle drying rack to place all of the parts is very handy. You also have the option to run parts and bottles through the dishwasher. A small dishwasher basket is helpful to keep small parts contained.
It is a general practice to sterilize pump parts and bottles before you use them for the very first time. Some parents make it a habit of sterilizing them periodically, but it is typically not necessary before each use. Your pediatrician may recommend that you sterilize bottles more frequently if your baby is born prematurely or has health considerations. If you plan to use a dishwasher, the dishwasher’s high temperature will sanitize the parts, and many models have a dedicated sterilize setting. If you handwash parts, there are electric steamers that will sterilize bottles, steam sterilizers that you put in your microwave, and sterilizers that use UV light. Plus, you can always place parts in a pot of boiling water for 10 minutes to sterilize them. If you have questions about sterilization, talk to your pediatrician. Some parents decide this is not necessary and skip sterilizing altogether.
One consideration for your method of cleaning or sterilization is that heat breaks down plastics. Products labeled “BPA-free” may still leach endocrine-disrupting chemicals like BPS or BPF when heated. Plus, there is evidence that exposure to high temperatures can significantly increase microplastic release. You can limit the exposure to heat by hand washing rather than using a dishwasher. Or if you choose to use a dishwasher, you may consider removing them to air dry rather than running through a heated dry cycle. The only method of sterilization that does not use heat is UV light. See this episode for more information on the safety of plastic baby bottles and alternatives.
Storing Breastmilk
For a healthy full-term baby, the guidelines for storing breastmilk are:
- 4-6 hours at room temperature
- 24 hours in a cooler with ice packs
- 3-8 days in the fridge
- 6-12 months in the freezer
The fresher the milk, the better. Over time, and with cooler temperatures, the properties in your milk will diminish. However, even milk that has been frozen for months still contains unique nutrients and immune properties that cannot be replicated in formula. Always follow storage guidelines and check dates before use.
You want a consistent system for labeling and organizing milk. You can combine milk from different pumping sessions, but only if it is at the same temperature. Do not add freshly pumped warm milk to cold milk from the refrigerator. If you plan to use milk soon, store it in the fridge. Label bottles or storage bags with the date, and if sending to daycare, also include your baby’s name.
You may also want to note the approximate time the milk was pumped. Research shows that breast milk changes throughout the day, with significant circadian variation in components such as tryptophan, fats, triacylglycerol, cholesterol, iron, melatonin, cortisol, and cortisone. These variations help regulate your baby’s sleep and circadian rhythms. If possible, give your baby milk pumped at roughly the same time of day they will consume it. That said, any pumped breast milk, regardless of timing, is still beneficial and preferable to formula when available.
Tips for Freezing and Thawing Breastmilk
If you plan to store milk for extended periods, freezing is the best option. There are a few simple strategies that can make it more efficient. Freeze milk in small portion sizes, typically 2–5 ounces (60–150 mL). Smaller portions thaw faster and reduce waste. For example, if you freeze only 5-ounce (150 mL) portions but your baby typically drinks 4 ounces, you will end up wasting an ounce at every feeding. By freezing smaller amounts, you can combine two bags if needed without wasting milk. For best results, use freezer bags specifically designed for breast milk storage. I recommend Lansinoh bags; I have used hundreds of these and they work wonderfully. When freezing, lay the bags flat. Once frozen, you can store them upright or in any position. Starting flat makes them easier to organize and allows you to fit more into a small freezer space.
To thaw frozen milk, place it in the refrigerator the night before you plan to use it, place the container under warm running water, or set it in a bowl of warm water. Avoid microwaving breast milk because microwaves can create dangerous hot spots, damage nutrients, and alter the milk’s composition.
Manage High Lipase in Stored Breastmilk
When thawing frozen breast milk, you may notice a change in smell or taste. This is often caused by lipase, an enzyme naturally present in breast milk. High lipase activity can give thawed milk a soapy or sour smell and taste. Some babies are unbothered, while others may refuse it. If your baby rejects milk due to high lipase levels, you can scald it before freezing. To do this, heat the milk in a small pot over the stove until tiny bubbles form around the edges (about 180°F / 82°C), then remove it from the heat, cool it, and freeze. Scalding prevents the off taste but can reduce some beneficial properties, so use fresh milk whenever possible.
Pumping and Storing Milk for NICU Babies
If your baby is admitted to the NICU, breast milk becomes even more critical for their nutrition, immune protection, and development. The NICU should be able to provide a hospital-grade pump, which can make pumping sessions faster and more efficient. Ask your NICU team about their storage protocols, labeling requirements, and whether you need to be more stringent with sterilizing pump parts. Many NICUs store milk in ultra-cold freezers (-70° to -80° C), which prevents the odor and taste changes from lipase that can occur in a standard home freezer over time.
Donate or Access Donor Breastmilk Safely
If your baby is in the NICU and you cannot provide enough milk, hospitals often source donor milk from milk banks. These organizations collect, screen, pasteurize, and distribute breast milk, prioritizing the most vulnerable infants. Donors go through health screenings, and all milk is tested before and after pasteurization to ensure safety. If you have extra milk that your baby will not use before it expires, donating it to a milk bank can make a significant difference for another family.
There are also informal milk-sharing networks that connect donors and recipients directly, though these are not regulated. You should be warned that not everyone seeking milk donations wants it for a baby. If you go this route, take precautions and work with your care provider or a lactation consultant to find reputable resources. Whether through a milk bank or direct sharing, donating milk helps give more babies access to the benefits of breast milk.
Planning to Pump at Work
Returning to work while breastfeeding often means that pumping becomes an essential part of your daily routine. Planning for all of the logistics will make the transition much smoother. The first few weeks back are an adjustment period as you settle into a new schedule. Give yourself time to adapt. It is a good idea to start pumping a few weeks before your return to build a small freezer stash. Having that reserve can relieve some of the pressure while you get comfortable with pumping on the job.
Communicate Your Pumping Needs at Work
Talk to your boss or HR department before returning to work to let them know you will need to pump breast milk during the day. This conversation can be awkward, but it doesn’t have to be. All you need to say is, “I will be providing breast milk for my baby when I return to work, and I will need to pump a few times a day.” If you prefer not to have the conversation in person, you can also send an email. Tailor your message to fit your workplace culture, but keep the tone confident and solution-oriented to convey that this will be happening, so let’s figure out the best way to make it work for everyone. Avoid framing it as a request, which could imply your boss has the option to say no.
In addition to talking with your employer, talk to coworkers who have been through pumping at work. They can be an excellent resource for understanding how your company handles it and can share practical tips on what worked well (and what did not) for them. If you are the first person in your workplace to go through it, take the opportunity to share your experience and help pave the way for those who come after you.
Plan Your Work Pumping Schedule
If your baby receives three bottles while you are at work, you should plan to pump three times. Typically, you will pump about every three hours during the workday. If you work 9-5, a common routine is to breastfeed in the morning before work, pump mid-morning, at lunch, and mid-afternoon. Then breastfeed your baby when you are reunited after work. On days off, you would breastfeed as usual without the need to pump
In the United States, employers are required to provide adequate time for pumping. However, they are not required to pay you during that time. One session will often fall during a lunch break. By the time you go back to work, you will be skilled at eating while pumping. The other sessions may be unpaid, depending on your company’s policy.
If your employer will not pay you for time spent pumping, look for ways to multitask during pumping. If you have a private office, you can continue your regular desk work. In shared spaces, you might review materials, make notes, or plan projects. You can also make phone calls, but be aware that pumps can be noisy. To reduce sound, place the pump further away, tuck it under a desk, or drape a towel or blanket over it. The tubing is usually long enough to give you some flexibility. With a bit of creativity, you can make your pumping time both productive and manageable.
Streamline Pumping Logistics at Work
Pumping at work involves more than just finding the time. You also need to manage your pumping space, take supplies back and forth, clean your equipment, and store your milk safely. The key is to make the process as simple and convenient as possible. The easier it is, the more likely you will be able to maintain your routine. If pumping becomes cumbersome, it can create another barrier to providing breastmilk for your baby.
Finding a Space to Pump
U.S. law requires employers to provide a private space for pumping that is not a bathroom. Your options will depend on your workplace. If you have a private office, you can pump without moving. If you are in a cubicle, privacy may be more challenging. Larger office buildings may have a dedicated lactation room or allow you to use an empty office or conference room. For other work environments such as retail, service, or warehouse settings, you may need to get creative. If you commute by car, your vehicle may be able to serve as a space to pump. Remember, pumping is temporary, so focus on solutions that work for now.
For peace of mind, you may want to ensure no one can walk in unexpectedly. In the workplace, place a sign on the door, such as “Baby’s lunch in progress” or a simple “Do not disturb.” If the room does not have a lock, you may consider requesting one from your employer or consider a portable lock or door security bar.
Toting and Storing Supplies
If you will be taking your pump and supplies to and from work or to another location during the day, consider how you will carry them. Breast pumps typically come with the basic unit and essential accessories, but not a tote bag. While breast pump manufacturers sell bags specifically designed for the pump and accessories, this is an additional and optional purchase. Any bag that fits your equipment can work. If you have a long commute, coolers and ice packs made for breast milk can be convenient, but a standard cooler is usually just as effective. If possible, consider keeping a spare set of supplies at work to avoid carrying everything back and forth. The key is finding a practical system within your budget.
Storing Milk at Work
After you pump, keeping milk chilled throughout the day is essential. Access to a fridge would be ideal. You could also use an insulated cooler with ice packs or an insulated thermos. Typically, you would keep milk chilled during the workday and take it home for use the next day. If your baby attends daycare, you can drop off milk for the following day when you pick them up. If you ever have more than your baby’s typical daily intake, you can freeze it.
Cleaning Pump Parts at Work
If you pump at work, you may need to get creative with your cleaning routine based on the space and resources available. One option is to place all pump parts in a sealed plastic bag and store them in the refrigerator between sessions, then wash them thoroughly at the end of the day. If you do not have access to a kitchen, you may need to use a bathroom sink. If you do not have a space to leave parts to air-dry, you may need to dry them by hand and store them with your pump.
Working in a shared space or using community resources can feel uncomfortable if you want to keep pumping private. While you should find solutions that make you feel at ease, remember that normalizing pumping benefits others, too. Your openness can help pave the way for future parents in your workplace. I encourage you to be open and proud about continuing to provide breastmilk for your baby even after you return to work.
How to Build a Stash
Whether you pump occasionally at home or every day at work, it is always nice to have some milk as a backup in your freezer. It is even possible to build a stockpile to continue providing breast milk even after you stop breastfeeding. Breast milk production works on a demand and supply system: the more milk you remove, the more your body will make. Once you have breastfeeding or pumping well established, you can use this principle to increase your supply and gradually build a freezer stash. Before you begin, consider why you want a stash and how much you actually need. A freezer full of milk may sound appealing, but it is not worth the effort if much of it will expire unused. Pumping takes time and energy, so set a realistic goal and reevaluate it as your needs change.
A good way to start is by pumping once a day after breastfeeding your baby, ideally after the first morning feeding when supply is often highest. For example, if your baby feeds at 6:00 AM, nurse first and then pump. You may only get a small amount at first. Consistency will signal your body to produce more milk at that time each day. Over time, even small amounts add up. Consider the following examples:
| Daily Pumped Amount | Total After 1 Month | Approx. Number of Feedings* |
| 2 oz (60 mL) | 60 oz (1.75 L) | ~12+ feedings |
| 4 oz (120 mL) | 120 oz (3.5 L) | ~24+ feedings |
*Based on a feeding of 5 oz (150 mL). If your baby drinks less, the stash will cover more feedings.
If you want to increase your supply even further, you could add an additional pumping session, beyond just pumping after feeding your baby.
Follow These Keys for Pumping Success
Whatever your pumping goals are, a few core principles will set you up for success.
Stick to a Routine
Consistent, regular milk removal is essential for maintaining supply. Aim to pump at relatively the same times each day, even on weekends. Avoid skipping sessions whenever possible. Skipped sessions can lead to a drop in supply that may be difficult to rebuild.
Plan for Your Pumping Time
Pumping takes more than just expressing milk; it also includes stepping away, setting up, and cleaning parts. Look ahead at your day and plan where those sessions will fit. If you are at work, you may need to coordinate with a co-worker, schedule breaks, or block out time on your calendar. It is easy to put off pumping when you are busy, you have to make it a priority.
Remember the Payoff
Pumping may feel inconvenient, but it will get easier and more efficient with time. Every session is an investment in your baby’s health. The time and effort you commit now will pay off in the long run.
Thank you to the brands that help power this podcast.
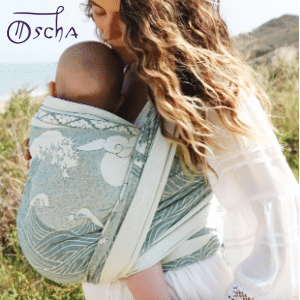
10% off Oscha Slings with the code PREGNANCYPODCAST
There are endless benefits to babywearing, from promoting bonding to giving you the ability to have your hands free as a busy parent. Oscha slings, wraps, and carriers are absolutely gorgeous and are ethically made in Scotland using the highest quality natural and organic yarns. From the newborn stage through toddlerhood, Oscha Slings are the most beautiful and comfortable solution for carrying your baby. New customers can get 10% off with the code PREGNANCYPODCAST.

Thank you to VTech for their support of this episode. VTech offers a wide range of baby monitors designed for today’s modern parents. As the #1 Baby Monitor Brand in North America, VTech is trusted by millions of families to deliver crystal-clear HD video, reliable performance, strong night vision, and convenient smartphone access. The Advanced HQ Max is built for parents who want an easy-to-use, secure monitor without the need for Wi-Fi or apps. With a large 7” screen and crisp, real-time video, it provides reliable monitoring without lag. The Advanced HQ Max is perfect if you want private, no-fuss monitoring with premium features. Click here to check out the Advanced HQ Max.

Track Your Fertility Hormones at Home with Inito
Inito is the first at-home fertility monitor that tracks four key fertility hormones (estrogen, LH, PdG, and FSH) all on a single test strip. In just ten minutes, you get accurate, personalized hormone data to help you understand your unique cycle and optimize your chances of conceiving. Inito is 96% as accurate as a blood test, without the cost, wait time, or hassle of going to a lab. If you are on a fertility journey, Inito provides you with clear insights into your unique hormone patterns, allowing you to stop guessing and start understanding your cycle more effectively. The Inito Starter Pack is available for just $89 with the code PREGNANCYPODCAST.
