Although your newborn is hard-wired to breastfeed, breastfeeding doesn’t always come naturally or go perfectly from the start. In reality, breastfeeding can take practice and patience as you and your baby navigate your nursing relationship. Many challenges can arise in the first few days and even months into your breastfeeding journey. The more you know about potential speed bumps, the better prepared you will be to address minor issues before they turn into bigger problems. Issues can include symptoms in your breasts like leaking, sore nipples, nipple shields, pain during breastfeeding or pumping, vasospasms, blebs, plugged ducts, mastitis, and engorgement. Or issues that affect your baby like jaundice, tongue-tie, thrush, food allergies or sensitivities, nursing strikes, cluster feeding, growth spurts, and spitting up. This episode will help you learn how to recognize and troubleshoot common breastfeeding challenges to make feeding your baby a more comfortable and successful experience.
Listen Now
This episode is made possible with support from our sponsors. I appreciate your support for the brands that help power this podcast.
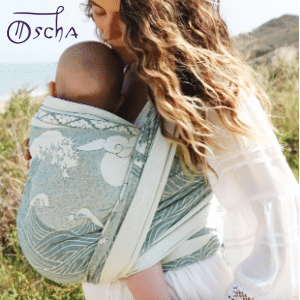
10% off Oscha Slings with the code PREGNANCYPODCAST. From the newborn stage through toddlerhood, Oscha Slings are the most beautiful and comfortable solution for carrying your baby.

Inito is the first at-home fertility monitor that tracks four key fertility hormones (estrogen, LH, PdG, and FSH) all on a single test strip. Inito is 96% as accurate as a blood test, without the cost, wait time, or hassle of going to a lab. The Inito Starter Pack is available for just $89 with the code PREGNANCYPODCAST.

VTech VM901 Baby Monitor makes monitoring effortless whether you’re at home or away. With a 1080p HD camera and a 5” parent unit, it’s designed for convenience and reliable performance. As the #1 Baby Monitor Brand in North America, VTech is trusted by millions of families. Click here to check out the VTech VM901 Baby Monitor.
Become a Pregnancy Podcast Premium member or log in to access all articles and episodes ad-free.
Article and Resources
I support the decisions you make for you and your baby when it comes to feeding. My goal is to provide accurate, evidence-based information and support to help you succeed. You can find all of the breastfeeding resources, episodes, and articles here.
The Value of a Lactation Consultant and Breastfeeding Support Groups
This episode is designed to help you understand and troubleshoot common breastfeeding issues, but it is not a substitute for personalized help. One of the best things you can do if you are struggling, or even if you have questions, is to seek support early. Addressing minor issues before they turn into bigger problems can make a huge difference in your breastfeeding experience.
An IBCLC, or International Board Certified Lactation Consultant, is specially trained to help you and your baby overcome challenges. They can assess feeding, provide hands-on guidance, and tailor solutions to your unique situation. While there may be a cost associated with working with a lactation consultant, many parents are surprised to find that their hospital, birth center, or insurance plan offers this support at little to no cost. If cost is a concern, your doctor, midwife, or pediatrician can often connect you with local, low-cost, or free resources.
In addition to one-on-one help, breastfeeding support groups can be an incredible resource. Connecting with other parents who are going through similar experiences can offer not just guidance, but a sense of community and reassurance. La Leche League is a wonderful place to start.
The Breastfeeding Relationship
Breastfeeding is more than just feeding; it is a relationship between you and your baby. For it to be successful, it needs to work for both of you. While your baby is born with instincts to breastfeed, challenges can still come up along the way. Some issues involve your breasts, and others show up in your baby’s behavior or feeding patterns. Having a basic understanding of common breastfeeding issues can help you feel more prepared. If something does come up, you will be more likely to recognize what is going on, know how to respond, and feel confident in getting help when you need it.
Breastfeeding Issues That Start With You
Let’s start by going over symptoms that can show up in you, and then we’ll move on to breastfeeding challenges that tend to present in your baby.
Leaking
Leaking is very common in the early days of breastfeeding as your body adjusts to your baby’s needs and your milk supply is still being regulated. If your breasts become full and you do not remove milk, they may leak. Leaking can also happen unexpectedly, for example, when you hear a baby cry or your let-down reflex is triggered.
If you are experiencing leaking, nursing pads can help absorb the excess milk and keep your clothes dry. There are two main types. Disposable pads are convenient, especially when you are on the go. They typically have an adhesive strip to keep them in place inside your bra and are designed to absorb moisture and wick it away from your skin. Washable nursing pads are a more environmentally friendly option. You can throw them in the washer and dryer and reuse them. One downside is that if they get wet, they may feel damp against your skin, unlike disposables, which tend to stay feeling dry.
Painful Latch
If your baby’s latch is painful, it is likely that they are not latched on properly. To safely remove your baby from your breast and try again, gently insert a finger into the corner of their mouth and turn it to break the suction. This allows you to unlatch them without pulling, which can be painful and cause nipple damage. If you find yourself doing this multiple times, it may feel frustrating, but in the long run, protecting your nipples is worth the effort.
When helping your baby latch, try the following tips. Gently tilt your nipple upward so the top points toward your baby’s upper lip. Wait for their mouth to open wide before bringing them to the breast. You can also gently compress your breast with your hand to make it easier for your baby to latch deeply. Be patient with yourself and your baby, and with consistency, it will get easier.
Sore Nipples
You may have heard that breastfeeding is not supposed to hurt. While that is true in the long term, it is very common to experience sore or sensitive nipples in the early days. This is a part of your body that is not used to such frequent stimulation, and some discomfort is normal as you and your baby adjust. That said, soreness is often a sign of a poor latch, and correcting the latch is the most crucial step to relieving and preventing further damage.
As you work on improving the latch, there are several things you can do to help your nipples heal. Babies usually suck more vigorously at the beginning of a feeding, so begin on the less sore side if one nipple is more irritated than the other. To promote healing, you can make a saline rinse with 8 ounces of warm water and ½ teaspoon of salt. Soak your nipples for about a minute after feeding, pat dry, and apply breastmilk to your nipple. Your milk has natural antibacterial and anti-inflammatory properties that can help with healing. You may also consider nipple cream to help soothe and heal your skin. Nipple creams or balms are best used short-term while you address the underlying cause.
If your nipples are chapped or cracked, using mild soap once daily can help keep the area clean without over-drying. Allow your nipples to air dry when possible. Damaged nipples can be painful, but they do heal. The more proactive you are in correcting latching issues as soon as possible, the more you can prevent problems like cracked nipples. You can visit the Kelly Mom blog for more info on Healing Tips for Nipple Cracks or Abrasions.
Nipple shields
Nipple shields are thin, flexible silicone covers worn over the nipple during breastfeeding. They can be helpful in specific situations, such as when a baby has difficulty latching or when you are experiencing nipple pain from cracks or other damage. While they can offer short-term relief or support, nipple shields are often misunderstood and sometimes misused.
For example, they may mask an underlying issue that needs to be addressed more directly, like a poor latch or a tongue-tie. Because of this, it is best to use a nipple shield under the guidance of a lactation consultant. An IBCLC can help ensure that a shield is the right solution for your specific situation, show you how to use it correctly, and create a plan for eventually weaning off of it if needed. If you want to read more about the pros and cons, including the potential difficulty of transitioning your baby away from a shield, check out this Kelly Mom article on the challenges of using a shield.
Pumping is Painful
Pumping should not be painful. If it is, there are a few things you can try to make it more comfortable and effective. First, check the suction level on your pump. Stronger suction does not always mean better results. Try lowering the suction to a more comfortable level.
Next, consider the flange size. Most pumps come with a standard flange, but one size does not fit all. The flange is the cone-shaped part that goes over your nipple. If it is too small or too large, it can cause discomfort. A nipple that is swollen or appears darker than usual after pumping may indicate an improper fit. It is normal for your nipple to be slightly enlarged after pumping, but it should not be painful or look bruised. Your nipple should move freely in and out of the flange during pumping. You can also try some olive oil to lubricate it and reduce friction.
Although it may seem like pumping and breastfeeding are separate skills, they are closely related. If you are experiencing issues with pumping, bottle feeding, or supplementing, a lactation consultant or a breastfeeding support group can be incredibly helpful.
Vasospasm or Nipple Blanching
If you experience a sharp, stinging, or burning sensation in your nipple, especially after a feeding, you might be dealing with a vasospasm. This is a sudden narrowing of the blood vessels, which temporarily reduces blood flow. A common visible sign of this is nipple blanching, where your nipple turns white during the spasm and then red or purple as the blood returns. Vasospasms usually happen after feeding, but can also occur between feedings. Some moms find that cold temperatures can trigger or worsen these episodes.
To stop a spasm in the moment, try gently squeezing the base of your nipple to help restore circulation. Keeping your nipples warm, especially after nursing, may help prevent future spasms. If you are experiencing these symptoms regularly, it is a good idea to talk to a lactation consultant or your care provider to rule out any other underlying causes, such as a latch issue or Raynaud’s phenomenon. For more details and practical strategies, see this Kelly Mom article on nipple blanching and vasospasms.
Blebs
A bleb, also known as a milk blister, is a small white or yellowish spot that can appear on the nipple. It usually looks like a tiny dot of milk is trapped in a pore. Blebs can sometimes cause pain during nursing, but not always. If a bleb is not bothering you, you do not need to treat it. If it is uncomfortable or persistent, there are a few remedies to treat it. Try a warm bath or shower, or soak the nipple in a cup of warm water mixed with two teaspoons of Epsom salt before nursing. You can soak a cotton ball in warm water, olive oil, or vinegar and place it in your bra.
If a bleb does not improve or is causing significant discomfort, reach out to a lactation consultant for additional support. For more detailed guidance, check out this Kelly Mom article on blebs and what you can do to treat them.
Low Milk Supply
Not making enough milk is one of the top reasons mothers start supplementing with formula and stop breastfeeding. Milk works on a demand and supply system; the more milk you remove from your breasts, the more milk your body will make. The number one thing you can do to increase your milk supply is to increase how often you feed your baby. While pumping is a great way to provide milk for your baby, a pump will not remove milk as effectively as your baby can.
Before you conclude that you are not making enough milk, ensure that it is the case. Please seek the help of a lactation consultant if you have concerns and want to continue breastfeeding. If your supply has decreased due to an underlying issue, you want to fix that issue, not just pump more throughout the day. Kelly Mom has an excellent article with many resources on increasing low milk supply.
Oversupply
On the opposite end of the spectrum of undersupply is oversupply. This may seem like a good problem, but it can create many other issues and make breastfeeding difficult. Oversupply may mean that you have a forceful let-down. This is when your milk comes out too quickly, which makes it difficult for your baby to nurse. Oversupply can also contribute to more severe problems like engorgement, plugged ducts, and mastitis.
Many moms who experience oversupply will notice a decrease by around three months. It is tricky to reduce supply without overdoing it and creating a problem with insufficient milk production. Kelly Mom has more information on oversupply and using herbs to reduce your milk supply. A lactation consultant can be invaluable for dealing with oversupply.
Engorgement
Engorgement happens when your breasts become overly full. This may occur when your milk first comes in or anytime you go too long between feedings. This can cause your breasts to feel hard, heavy, tender, or even hot to the touch. Engorgement can also make it more difficult for your baby to latch.
The best way to relieve engorgement is to nurse your baby. If your breasts are too firm and your baby is struggling to latch, try using reverse pressure softening. This involves using your fingertips to gently press around your areola to move some of the fluid back into the breast, making the area around your nipple softer and easier for your baby to latch. For step-by-step instructions and helpful visuals, check out this Kelly Mom article on reverse pressure softening.
You can also express a small amount of milk by hand or with a pump to soften your breasts enough for a more comfortable latch. Just keep in mind that breastfeeding works on a demand and supply system. Fully emptying your breasts when you are already engorged may signal your body to make even more milk, potentially leading to more issues. A warm shower can help get your milk flowing for hand expression. While heat can assist with milk release, cool compresses are often more effective at relieving the discomfort and inflammation associated with engorgement. For more information on engorgement, see this Kelly Mom article.
Plugged Duct
Your breasts contain many ducts that transport milk to your nipple. When one of those ducts becomes blocked, it cannot fully empty, which can lead to a plugged duct. You might notice a firm, tender lump in your breast that feels swollen, warm, or even painful to the touch. Plugged ducts often result from inefficient milk removal if your baby is not nursing effectively or if you go too long between feedings. You can also cause a plugged duct with a bra that is too tight or doesn’t fit well.
To help clear a plugged duct, keep feeding or pumping regularly to encourage milk flow. Apply heat before nursing with a warm compress or shower. Gently massage the area during feedings, working from the plugged spot toward your nipple.
Mastitis
If you do not resolve a plugged duct, it can lead to mastitis, which is inflammation of the breast tissue. The symptoms are similar to a plugged duct but often more intense and may include redness or swelling, as well as flu-like symptoms like fever, chills, and aches. Mastitis may include an infection if bacteria enter through a point of damage on the nipple. Treatment typically includes the same steps as for a plugged duct, and you also want to rest, preferably in bed, with your baby. If you have a fever or flu-like symptoms, contact your doctor or midwife. Your care provider may prescribe antibiotics if they suspect an infection. For a detailed comparison of plugged ducts and mastitis, check out this helpful Kelly Mom article.
Weakened immunity is one risk factor for mastitis. I got mastitis with my son, and it was not fun. When I breastfed my daughter, I experienced it again, but that time, it progressed into a full-blown abscess. That was a whole new level of not fun. If you want to hear more about that journey and what the lessons learned breastfeeding the second time around. Taking care of your overall health is incredibly important, especially in the first few weeks postpartum when mastitis is most common. If you do anything that helps support or boost your immune system, now is the time to make it a priority. For me, that includes plenty of rest and daily AG1.
Breastfeeding Issues That Show Up in Your Baby
Now that we have covered symptoms that can show up in you, let’s move on to breastfeeding challenges that show up in your baby.
Spitting up
Spitting up is very common in babies. This is why most new parents keep a burp cloth close by at all times. While it can look dramatic, it usually does not bother your baby and often appears to be more than it is. In most cases, it is entirely normal and nothing to worry about. Spitting up is not the same as vomiting. Spitting up is usually a gentle, effortless flow of milk from the mouth. Vomiting involves a forceful expulsion of stomach contents and may be a sign of illness.
Thankfully, there are some simple things you can try to help reduce the amount your baby spits up. First, burp your baby after each feeding to release any swallowed air. Keep them upright for a little while after feeding rather than lying them down immediately. If you’re concerned about how often your baby is spitting up or whether it might be reflux or something more, talk to a lactation consultant or your pediatrician. For more on this topic, including signs of reflux and strategies to manage it, check out this article from Kelly Mom.
Sleepy Baby
In the early days of breastfeeding, it is essential to establish a strong feeding routine. This can be tricky if your baby tends to fall asleep at the breast or is very overly sleepy in general. To support healthy weight gain, it is typically recommended to wake your baby to feed every 2–3 hours during the day and every 4 hours at night, at least until they regain their birth weight. Always check with your doctor, midwife, or pediatrician for personalized guidance on how often to feed your baby.
If your baby dozes off during feedings, there are gentle ways to keep them awake and engaged. Try burping them partway through the feeding. You can change their diaper, undress them slightly, or shift positions to stimulate alertness. Use skin-to-skin contact, which can also promote more active feeding. Some babies are just naturally sleepier than others, and that is okay. With time and consistency, most babies become more efficient and alert during feedings. For more tips, see this article on sleepy babies from Kelly Mom.
Nursing Strikes
A nursing strike happens when your baby suddenly refuses to breastfeed. The keyword here is suddenly. This is not the same as weaning, which typically happens gradually and rarely occurs on its own before age two. Nursing strikes can happen for a wide range of reasons. It could be something obvious, like a cold or teething. It could also be something more obscure, such as a change in the taste of your milk. Whatever the cause, a strike can be stressful, but it is almost always temporary.
The good news is that there are many tips for navigating a nursing strike. First, continue expressing milk by hand or with a pump to maintain your supply and avoid plugged ducts. Do not try to force breastfeeding because it can create more stress for both you and your baby. Your baby may be more relaxed and willing to latch when they are sleepy or just waking up. Experiment with different positions or locations. A change of scenery or posture might help reset the routine. Most nursing strikes resolve with time, patience, and continued encouragement. For more suggestions and support, check out the Kelly Mom article, aptly titled, Help My Baby Won’t Nurse.
Cluster Feeding and Growth Spurts
On the opposite end of a nursing strike is a baby who seems like they will not stop nursing. This can be frustrating at times, but this is normal. Feeding patterns can vary a lot, especially in the early weeks and months. Cluster feeding occurs when your baby nurses more frequently during a specific window of time. For example, if they want to nurse nearly nonstop from 5–8 PM, that is cluster feeding. This often happens in the evening, when babies tend to be fussier and seek extra comfort. Your breast is their safe space, and nursing is physically and emotionally soothing. You can read more on Kelly Mom if you are dealing with a fussy baby in the evenings and cluster feeding.
Another reason your baby may seem hungrier than usual is a growth spurt. These often show up as increased feeding and fussiness and typically last a few days, although some can stretch up to a week. Common times for growth spurts include: 2–3 weeks, 4–6 weeks, 3, 4, 6, and 9 months. Every baby is different, so your experience may not follow this exact timeline. It can be exhausting in the moment, but have some appreciation for how amazing it is that your body can increase milk supply to meet your baby’s growing needs. Kelly Mom offers more information on growth spurts in this article.
Food Allergies and Sensitivities
You pass everything you eat to your baby in trace amounts through your breast milk. For most babies, this is not an issue. In some cases, your baby may have a food allergy or sensitivity that causes symptoms. Possible signs of a sensitivity include: fussiness or irritability, spitting up more than usual, excess gas, a rash on the cheeks or bottom, or Eczema-like patches.
The only real way to determine whether something in your diet is bothering your baby is through elimination. You have to remove the suspected food and see if symptoms improve. Keep in mind that it may take one to two weeks after eliminating a food to see noticeable changes. Common foods associated with allergies or intolerances include: cow’s milk (not just milk itself but also cheese, butter, and many processed foods), soy, eggs, wheat, and corn. This can be a challenging process of trial and error, and it may be helpful to work with your pediatrician, a lactation consultant, or a dietitian if you suspect a food sensitivity. For more information on dairy and food sensitivities, check out this article on Kelly Mom.
Tongue Tie and Lip Tie
Tongue-tie occurs when the frenum or frenulum (the small membrane under your baby’s tongue) is too short or tight, restricting the tongue’s movement. Because babies use their tongues to latch and draw milk effectively, a tongue-tie can interfere with breastfeeding and lead to issues like poor latch and difficulty feeding. A lip-tie is a similar condition where the membrane connecting the upper lip to the gums is too tight. This can also impact your baby’s ability to latch deeply and create a good seal while nursing.
While you might be able to spot a restriction yourself, diagnosis and treatment should come from a pediatrician, dentist familiar with oral ties, or a lactation consultant. Signs of a tongue-tie or lip-tie may include difficulty maintaining a latch or struggling to suck or swallow effectively. You may also notice clicking sounds while nursing, excessive gassiness or fussiness during feeds, poor weight gain, or nipple pain or damage.
Treatment usually involves a simple procedure called a frenotomy or frenectomy, where the membrane is clipped or released. It is typically quick, done with local anesthetic, and recovery is fast. If your baby is diagnosed with a tie, addressing it early can make a big difference in breastfeeding success. You can read this article on Kelly Mom for additional resources for breastfeeding a baby with tongue-tie or lip-tie.
Yeast Infection and Thrush
Yeast infections can affect both you and your baby during breastfeeding, and when this happens, it is often referred to as thrush. Thrush is caused by an overgrowth of Candida, a type of yeast that thrives in warm, moist environments. In you, a yeast infection may cause your nipples to appear pink, shiny, or flaky, and you might experience burning, itching, or pain. In your baby, thrush often shows up as creamy white patches in the mouth or on the tongue that do not wipe off easily. It is common for babies to have a white coating on their tongue from milk, but that should come off with gentle wiping.
Thrush can be passed back and forth between you and your baby, which makes it particularly stubborn to treat. If you suspect thrush, contact your doctor, midwife, or a lactation consultant. Treatment typically involves antifungal medication for both you and your baby. It is also essential to clean and sanitize anything that comes into contact with your nipples or your baby’s mouth, like pacifiers, bottle nipples, breast pump parts, and even nursing bras. For more detailed guidance, visit this Kelly Mom article with additional thrush resources.
Jaundice
Jaundice occurs when there is a buildup of a substance called bilirubin in your baby’s blood. Bilirubin is produced naturally as the body breaks down red blood cells, and the liver is responsible for removing it from the bloodstream. In newborns, the liver is still maturing and may not process bilirubin efficiently, which can result in a yellowish tint to the skin.
It is very common for babies to have a mild case of jaundice in the first few days of life. In most cases, it is harmless and resolves on its own. However, if bilirubin levels become too high, jaundice can lead to more serious health problems. Jaundice tends to be more common in breastfeeding newborns, especially those who are not nursing effectively. One of the best ways to help prevent or manage jaundice is to breastfeed frequently, ideally eight to twelve times per day during the first few days. This supports milk production and helps your baby pass bilirubin more efficiently.
If you suspect your baby has jaundice, contact your pediatrician. It typically first appears on the face and then moves downward to the chest, abdomen, arms, and legs. The whites of the eyes may also appear yellow. Your pediatrician will check for signs of jaundice at your baby’s early visits and may order a skin or blood test to confirm a diagnosis if needed.
Jaundice usually peaks around three to five days after birth. If treatment is necessary, it may involve light therapy to help lower bilirubin levels. This treatment can be in the hospital or at home, depending on the severity. For more information on breastfeeding a baby with jaundice, visit this article from Kelly Mom.
Final Note
Breastfeeding can be a beautiful and rewarding experience, but it is not always easy. There are many common challenges, and most are manageable with the correct information and support. If you take one thing away from this episode, almost every breastfeeding issue has a solution. The sooner you can identify what is going on and get support, the easier it is to get back on track and continue your breastfeeding journey and reach your breastfeeding goals.
Additional Resources:
- The Womanly Art of Breastfeeding: This is a complete guide on everything from the moment your baby is born until the end of your breastfeeding relationship. I have personally read this book numerous times and referenced it many times throughout my own breastfeeding experiences. As a disclaimer, it is extensive and leans heavily toward exclusive breastfeeding without formula supplementation.
- Pregnancy Podcast Breastfeeding Resources: All of the Pregnancy Podcast episodes, articles, and resources for breastfeeding in one place.
- La Leche League: An international organization with many free local and online resources and support groups.
- Kelly Mom blog: An excellent resource for breastfeeding-related topics and expert advice.
Thank you to the brands that help power this podcast.
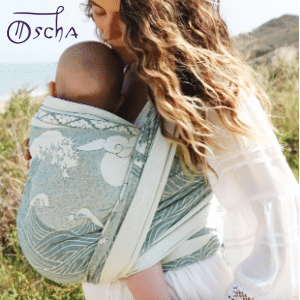
10% off Oscha Slings with the code PREGNANCYPODCAST
There are endless benefits to babywearing, from promoting bonding to giving you the ability to have your hands free as a busy parent. Oscha slings, wraps, and carriers are absolutely gorgeous and are ethically made in Scotland using the highest quality natural and organic yarns. From the newborn stage through toddlerhood, Oscha Slings are the most beautiful and comfortable solution for carrying your baby. New customers can get 10% off with the code PREGNANCYPODCAST.

Track Your Fertility Hormones at Home with Inito
Inito is the first at-home fertility monitor that tracks four key fertility hormones (estrogen, LH, PdG, and FSH) all on a single test strip. In just ten minutes, you get accurate, personalized hormone data to help you understand your unique cycle and optimize your chances of conceiving. Inito is 96% as accurate as a blood test, without the cost, wait time, or hassle of going to a lab. If you are on a fertility journey, Inito provides you with clear insights into your unique hormone patterns, allowing you to stop guessing and start understanding your cycle more effectively. The Inito Starter Pack is available for just $89 with the code PREGNANCYPODCAST.

VTech offers a wide range of baby monitors designed for today’s modern parents. As the #1 Baby Monitor Brand in North America, millions of families trust VTech to deliver crystal-clear HD video, reliable performance, strong night vision, and convenient smartphone access. The VTech VM901 Baby Monitor makes monitoring effortless whether you’re at home or away. With a 1080p HD camera and a 5” parent unit, it’s designed for convenience and reliable performance. As the #1 Baby Monitor Brand in North America, VTech is trusted by millions of families. Click here to check out the VTech VM901 Baby Monitor.
